Contained power morcellation within an insufflated isolation bag
OBJECTIVE
To describe a technique for contained power morcellation within an insufflated isolation bag at the time of uterine specimen removal during minimally invasive gynecologic procedures.
METHODS
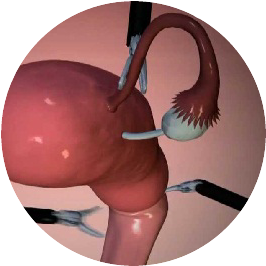
Over the study period of January 2013 to April 2014, 73 patients underwent morcellation of the uterus or myomas within an insufflated isolation bag at the time of minimally invasive hysterectomy or myomectomy. This technique involves placing the specimen into a large plastic bag within the abdomen, exteriorizing the opening of the bag, insufflating the bag within the peritoneal cavity, and then using a power morcellator within the bag to remove the specimen in a contained fashion. Procedures were performed at four institutions and included multiport laparoscopy, single-site laparoscopy, multiport robot-assisted laparoscopy, or single-site robot-assisted laparoscopy. Demographic and perioperative characteristics were collected for the cases.
RESULTS
Surgical specimen morcellation within an insufflated isolation bag was successfully used in all cases. The median operative time was 114 minutes (range 32-380 minutes), median estimated blood loss was 50 mL (range 10-500 mL), and the median specimen weight was 257 g (range 53-1,481 g). There were no complications related to the contained morcellation technique nor was there visual evidence of tissue dissemination outside of the isolation bag.
CONCLUSION
Morcellation within an insufflated isolation bag is a feasible technique. Methods for morcellating uterine tissue in a contained manner may provide an option to minimize the risks of open power morcellation while preserving the benefits of minimally invasive surgery.
Sydney Contained in Bag Morcellation for Laparoscopic Myomectomy
Abstract STUDY OBJECTIVE To demonstrate a new technique of contained in bag morcellation of a myoma after laparoscopic myomectomy. DESIGN Step-by-step explanation of the technique in a narrated video. INTERVENTION Contained In Bag Morcellation of myoma after laparoscopic myomectomy. MEASUREMENTS AND MAIN RESULTS Recent controversy regarding the risk of disseminating occult leiomyosarcomatous tissue during morcellation means we need to revise our current approach to tissue extraction at laparoscopic myomectomy and morcellation in general. Herein we present a novel technique, conceived by Dr. Danny Chou, called the Sydney Contained In Bag Morcellation technique for laparoscopic myomectomy. In this technique an EndoCatch bag (EndoCatch II Auto Suture Specimen Retrieval Pouch; Covidien, Mansfield, MA) is introduced in the typical fashion, the myoma is retrieved, and the mouth of the bag is exteriorized onto the abdominal wall. A 12-mm trocar is then introduced within the bag, and pneumoperitoneum is created before introducing an optical balloon tip port (KII Balloon Blunt Tip System; Applied Medical, Rancho Santa Margarita, CA) and the power morcellator device. Morcellation is then performed within the bag, under direct vision. This technique may offer a safer approach to morcellation because the bowel is not within the morcellation field and there is lower risk of disseminating occult leiomyosarcomatous tissue during morcellation. Subsequent to the morcellation process, suctioning of the bag removes any aerosolized particles of myoma, further minimizing the risk of possible dissemination. KNOW MORECONCLUSION
This technique may enable a minimally invasive approach to myomectomy to continue as a viable option in the era since the warning by the US Food and Drug Administration.The Sydney Contained In Bag Morcellation technique.
CONCLUSION
The Sydney Contained in bag Morcellation technique offers a possible solution to the risk of dissemination of benign morcellated and potentially leiomyosarcomatous myoma fragments. Certain aspects of the procedure are key to its success. The stay sutures are essential to facilitate orientation and opening of the bag mouth. The McCartney tube enables easier insertion of the flaccid bag into the vagina, and the suture-retaining slits enable the mouth of the bag to be opened quickly and easily. We have used this technique in 5 cases with uteri ranging in weight from 350 to 978 g. Recently, similar techniques have been described for use in single-port surgery and conventional laparoscopy [1,2]. Our technique is suitable for use with large uteri after total laparoscopic hysterectomy because the large capacity of the bag enables containment of uteri that would exceed the capacity of manually deployed specimen retrieval bags. This technique offers an alternative to vaginal morcellation, with the advantage of improved vision during morcellation and the ability to morcellate large uteri using a familiar instrument and view.Risk of leakage and tissue dissemination with various contained tissue extraction (CTE) techniques: an in vitro pilot study.
Abstract
STUDY OBJECTIVE
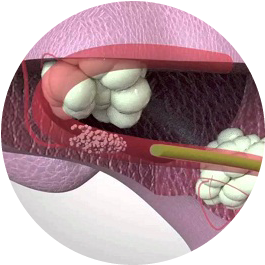
To evaluate risk of leakage and tissue dissemination associated with various contained tissue extraction (CTE) techniques.DESIGN
In vitro study (Canadian Task Force classification: II-1).SETTING
Academic hospital simulation laboratory.INTERVENTION
Beef tongue specimens weighing 400 to 500 g were stained using 5 mL indigo carmine dye and morcellated under laparoscopic guidance within a plastic box trainer. CTE was performed via 3 different techniques: a stitch-sealed rip-stop nylon bag and multi-port approach; a one-piece clear plastic 50 × 50-cm isolation bag and multi-port approach; or a 1-piece clear plastic 50 × 50-cm isolation bag and single-site approach. Four trials of each CTE method were performed and compared with an open morcellation control. All bags were insufflated to within 10 to 25 mmHg pressure with a standard CO2 insufflator. Visual evidence of spilled tissue or dye was recorded, and fluid washings of the box trainer were sent for cytologic analysis.MEASUREMENTS AND MAIN RESULTS
Blue dye spill was noted in only 1 of 12 CTE trials. Spillage was visualized from a seam in 1 of the 4 stitch-sealed rip-stop nylon bags before morcellation of the specimen. The only trial in which gross tissue chips were visualized in the box trainer after morcellation was the open morcellation control. However, cytologic examination revealed muscle cells in the open morcellation washings and in the washings from the trial with dye spill. Muscle cells were not observed at cytologly in any of the other samples. KNOW MORECONCLUSION
CTE did not result in any leakage or tissue dissemination with use of the single-site or multi-port approach when using a 1-piece clear plastic 50 × 50-cm isolation bag. Further studies are needed to corroborate these findings in an in vivo context and to evaluate use of alternate bag options for specimen containment.Assessment of the physical properties of endoscopic retrieval systems.
Abstract
BACKGROUND
A reliable method of retrieval of laparoscopically resected organs is required. The physical properties of three commercial systems available for clinical use (two plastic, one woven fabric) were examined.METHODS
Pig abdominal walls and gallbladders containing steel balls to represent gallstones were used to simulate organ retrieval on 60 occasions. The performance of retrieval bags was measured in terms of the temporal profile of pressure developed inside the bag, the force on the bag during withdrawal, and whether or not the bag could be retrieved intact. The force versus elongation relationship was also determined for each bag.RESULTS
Although there was a wide range of maximum pressures recorded (14-320 mmHg) with each retrieval system, the mean pressures in the plastic systems were significantly higher. The forces recorded during attempted withdrawal of both plastic bags were significantly lower than those with the fabric system (BERT bag: mean (range) 87 (25-165) N; Endocatch: 40 (7-123) N; Endopouch: 40 (14-68) N; P = 0.005 Endocatch versus BERT, P = 0.004 Endopouch versus BERT). The BERT bags tore more easily at the site of the grasper. KNOW MORECONCLUSION
Plastic retrieval systems were less likely to burst than fabric systems when subjected to simulated retrieval, and required less force for withdrawal. Plastic systems may therefore be associated with less tumor seeding or gallstone spillage as a consequence of bag disruption.In-Bag Morcellation
Abstract
In-bag morcellation seems to be a viable alternative to open power morcellation and offers the advantage of minimal to no spillage of tissue or fluids during morcellation. We report our initial experience and technique using this approach. KNOW MOREAlterations in Surgical Technique Following FDA Statement on Power Morcellation.
OBJECTIVE
Electromechanical morcellation (EMM), commonly known as “power morcellation”, often allows patients the benefits of minimally invasive surgical (MIS) approaches including decreased morbidity and mortality. 1 However, the role of EMM in myomectomy and hysterectomy has recently come under scrutiny due to concerns of heightened risks of intraperitonieal cancer dissemination in women with occult malignancies. In November 2014, the U.S. Food and Drug Administration (FDA) issued a safety warning for using EMM to remove uterine fibroids2. Despite prevalent public debate, it is unclear whether and how gynecologic surgeons have changed their practice. The current study seeks to assess influence of the FDA warning regarding EMM on management strategies in hysterectomies / myomectomies.
DESIGN
We conducted an online survey of American Association of Gynecologic Laparoscopists Minimally Invasive Gynecology Surgery Fellowship program faculty during December 2014-February 2015 using the Qualtrics Survey Tool (Qualtrics, Provo, UT). Email addresses were obtained from fellowship program’s websites. Of the 189 faculty, 40 were undeliverable, resulting in an effective target population of 161 faculty members. Survey questions were developed based on literature review and expert opinion, and pilot-tested on a convenience sample of gynecologic surgeons before final implementation.
RESULTS
Forty-six faculty completed the survey (response rate=29%). Of these respondents, 62% were male, 60% had over 10 years of experience, 60% were in gynecology-only practices, and 67% performed more than 50 hysterectomies / myomectomies annually. Although 28 respondents (61%) said they have never diagnosed leiomyosarcoma, 12 (26%) encountered at least one patient in 2013 with occult malignancy during a benign procedure. Forty-three surgeons (93%) reported using morcellation during hysterectomies / myomectomies in 2013, with uncontained EMM being the most commonly used form (81%). Table 1 summarizes practice changes in these 43 surgeons. Thirty-six (78%) noted that they changed their surgical approach for hysterectomies / myomectomies after the FDA warning. Of them, 21 (58%) used minilaporotomy, 18 (50%) used specimen retrieval pouches, and 15 (42%) used vaginal extraction in a bag, while 14 (39%) reduced the use of laparoscopic supracervical hysterectomy and 9 (25%) changed the route of hysterectomy to total laparoscopic or total abdominal hysterectomy.
CONCLUSION
Prior to the FDA warning, EMM was commonly used in hysterectomies / myomectomies. However, gynecologic surgeons have since adopted a variety of changes to their management strategies. Variations in preoperative evaluation demonstrates an inability to definitely diagnose malignancy preoperatively. 5 The large proportion of respondents who now use larger incisions or open procedures raises concern about potentially higher patient morbidity. Safety, efficiency, and long-term outcome data for the innovative surgical techniques that have been adopted (e.g., various containment bags, vaginal incisions, and intraoperative biopsies) are urgently needed. Further research on the prevalence of occult uterine cancer in women undergoing hysterectomies / myomectomies for presumed benign indications and their prognosis after EMM will also facilitate discussion on optimal management approaches, as our current knowledge is largely based on studies with small sample sizes and non-representative samples.3,4 Efforts to prevent cancer dissemination must be balanced with the lost benefits of MIS and potential risk of newly adopted yet understudied surgical techniques.
Complete plastic lining of the abdominal cavity during laparoscopic electromechanical morcellation-a promising technique
Abstract
The risk of intraperitoneal fragment dissemination of uterine tissue, especially the dissemination of unexpected leiomyosarcoma during electromechanical morcellation, has been increasingly debated during the last year. An improved technique for contained morcellation of uterine tissue inside an insufflated plastic bag during laparoscopy is presented. Twenty-one consecutive contained morcellations were carried out during the summer of 2014, at one institution. Five laparoscopic myomectomies and 16 hysterectomies were performed. Standard laparoscopic equipment was used and a transparent plastic bag was introduced into the abdominal cavity through the umbilical incision mounted on two curved blunt metal probes, which facilitated the placement of the uterine tissue into the bag. Morcellation was carried out inside the plastic bag through the opening in the umbilicus. All 21 morcellations during the study period were successfully performed. The median operative time was 105 min (range 45-180 min) and applying plastic bag and trocar median 10 min (range 4-30 min). Median specimen weight was 560 g (range 80-1265 g). No complications occurred, and no unintended bag perforation was identified. The presented improved contained morcellation technique is feasible in laparoscopic hysterectomy and myomectomy. Larger studies will however be required before the general introduction of the method.
KNOW MORETissue removal utilizing Steiner Morcellator within a LapSac: effects of a fluid-filled environment.
Abstract
BACKGROUND AND PURPOSE
Tissue removal can be a simple process of withdrawal of the entire organ, piecemeal removal with surgical clamps, or mechanical morcellation. Different mechanical morcellators exist that each have advantages and disadvantages. We have investigated a particular morcellator having an internal mechanized blade system that increases the chances of damage to tissue isolation sacks but removes large volumes of intact organ that can more readily be evaluated histologically. The primary premise of this investigation is that a fluid-filled sack would be less likely to be damaged by the activated blades of the morcellator.
MATERIALS AND METHODS
Utilizing a Steiner Morcellator (Karl Storz, Culver City, CA), two porcine kidneys were morcellated within the large LapSac (Cook Urological, Spencer, IN). Two environmental variables were evaluated: dry sac morcellation and fluid-filled sac morcellation. Each session was timed, fluid leakage identified, grasping of the sacks quantified, and gross spillage noted. The tissues were submitted for pathologic evaluation to quantify any differences grossly or histologically. All LapSacs were inspected for gross violation and inflated to distention with fluid to check for tiny leaks.
RESULTS
The Steiner Morcellator worked much better within the confines of the LapSac filled with fluid. There were no perforations in our experimental setting. It was not possible discern use of fluid-filled sacks histologically.
CONCLUSION
The Steiner Morcellator can be utilized safely in the LapSac if cautious observation and fluid-filled sack conditions are maintained. The extracted tissue is easily evaluated histologically.
Options on fibroid morcellation: a literature review
Abstract
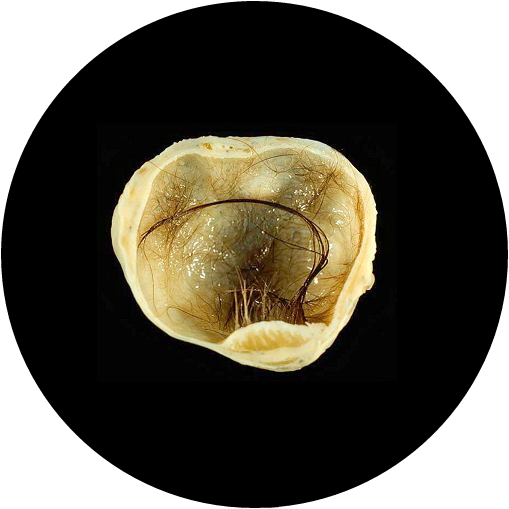
BACKGROUND AND PURPOSE
In laparoscopy, specimens have to be removed from the abdominal cavity. If the trocar opening or the vaginal outlet is insufficient to pass the specimen, the specimen needs to be reduced. The power morcellator is an instrument with a fast rotating cylindrical knife which aims to divide the tissue into smaller pieces or fragments. The Food and Drug Administration (FDA) issued a press release in April 2014 that discouraged the use of these power morcellators. This article has the objective to review the literature related to complications by power morcellation of uterine fibroids in laparoscopy and offer recommendations to laparoscopic surgeons in gynaecology. This project was initiated by the executive board of the European Society of Gynaecological Endoscopy. A steering committee on fibroid morcellation was installed and experienced ESGE members requested to chair an action group to address distinct clinical questions. Clinical questions were formulated with regards to the sarcoma risk in presumed uterine fibroids, diagnosis of sarcoma, complications of morcellation and future research. A literature review on the different subjects was conducted, systematic if appropriate and feasible. It was concluded that the true prevalence of uterine sarcoma in presumed fibroids is not known given the wide range of prevalences (0.45–0.014 %) from meta-analyses mainly based on retrospective trials. Age and certain imaging characteristics such as ‘lacunes’ suggesting necrosis and increased central vascularisation of the tumour are associated with a higher risk of uterine sarcoma, although the risks remain low. There is not enough evidence to estimate this risk in individual patients. Complications of morcellation are rare. Reported are direct morcellation injuries to vessels and bowel, the development of so-called parasitic fibroids requiring reintervention and the spread of sarcoma cells in the abdominal cavity, which may possibly or even likely upstaging the disease. Momentarily in-bag morcellation is investigated as it may possibly prevent morcellation complications. Because of lack of evidence, this literature review cannot give strong recommendations but offers only options which are condensed in a flow chart. Prospective data collection may clarify the issue on sarcoma risk in presumed fibroids and technology to extract tissue laparoscopically from the abdominal cavity should be perfected.
Use of Electric Power Morcellation and Prevalence of Underlying Cancer in Women Who Undergo Myomectomy
Abstract
IMPORTANCE
Myomectomy, the excision of uterine leiomyoma, is now commonly performed via invasive surgery. Electric power morcellation, or fragmentation of the leiomyoma with a mechanical device, may be used to facilitate extraction of the leiomyoma.
OBJECTIVE
To analyze the prevalence of underlying cancer and precancerous changes in women underwent myomectomy with and without electric power uterine morcellation.
DESIGN, SETTING AND PARTICIPANTS
We used a US nationwide database to retrospectively women who underwent myomectomy at 496 hospitals from January 2006 to December 2012. Use of electric power morcellation at the time of myomectomy was investigated. The prevalence of uterine cancer, uterine neoplasms of uncertain malignant potential, and endometrial hyperplasia were estimated. Multivariable mixed-effects regression models were developed to examine predictors of use of electric power morcellation and factors associated with adverse pathologic outcomes.
MAIN OUTCOMES AND MEASURES
Use of electric power morcellation at the time of myomectomy examined. The occurrence of uterine cancer and precancerous uterine lesions was determined.
RESULTS
The cohort consisted of 41 777 women who underwent myomectomy at 496 included 3220 (7.7%) who had electric power morcellation. Uterine cancer was identified in 73 (1 in 528) women who underwent myomectomy without electric power morcellation (0.19%; 95% CI, 0.15%-0.23%) and in 3 (1 in 1073) women who underwent electric power morcellation (0.09%; 95% CI, 0.02%-0.27%). The corresponding rates of any pathologic finding (cancer, tumors of uncertain malignant potential, or endometrial hyperplasia) were 0.67% (n = 257) (95% CI, 0.59%-0.75%) (1 in 150) and 0.43% (n = 14) (95% CI, 0.21%-0.66%) (1 in 230), respectively. Advanced age was the strongest risk factor for uterine cancer.
CONCLUSIONS AND RELEVANCE
The prevalence of cancers and precancerous abnormalities of the uterus in women who undergo myomectomy with or without electric power morcellation is low overall, but risk increases with age. Electric power morcellation should be used with caution in older women undergoing myomectomy.
Laparoscopic hysterectomy with morcellation vs abdominal hysterectomy for presumed fibroid tumors in premenopausal women: a decision analysis
OBJECTIVE
The purpose of this study was to model outcomes in laparoscopic hysterectomy with morcellation compared with abdominal hysterectomy for the presumed fibroid uterus and to examine short- and long-term complications and death.
STUDY DESIGN
A decision tree was constructed to compare outcomes for a hypothetical cohort of 100,000 premenopausal women who underwent hysterectomy for presumed fibroid tumors over a 5-year time horizon. Parameter and quality-of-life utility estimates were determined from published literature for postoperative complications, leiomyosarcoma incidence, death related to leiomyosarcoma, and procedure-related death.
RESULTS
The decision-tree analysis predicted fewer overall deaths with laparoscopic hysterectomy compared with abdominal hysterectomy (98 vs 103 per 100,000). Although there were more deaths from leiomyosarcoma after laparoscopic hysterectomy (86 vs 71 per 100,000), there were more hysterectomy-related deaths with abdominal hysterectomy (32 vs 12 per 100,000). The laparoscopic group had lower rates of transfusion (2400 vs 4700 per 100,000), wound infection (1500 vs 6300 per 100,000), venous thromboembolism (690 vs 840 per 100,000) and incisional hernia (710 vs 8800 per 100,000), but a higher rate of vaginal cuff dehiscence (640 vs 290 per 100,000). Laparoscopic hysterectomy resulted in more quality-adjusted life years (499,171 vs 490,711 over 5 years).
CONCLUSION
The risk of leiomyosarcoma morcellation is balanced by procedure-related complications that are associated with laparotomy, including death. This analysis provides patients and surgeons with estimates of risk and benefit on which patient-centered decisions can be made.